Potential Risks from Arsenic in the Maternal Diet – Additional Information on Epigenetic Effects
On this page
Skip the menu of subheadings on this page.This is a paper for discussion.
This does not represent the views of the Committee and should not be cited.
Introduction
1. The Scientific Advisory Committee on Nutrition (SACN) last considered maternal diet and nutrition concerning offspring health in its reports on ‘The influence of maternal, fetal and child nutrition on the development of chronic disease in later life’ (SACN, 2011) and on ‘Feeding in the first year of life’ (SACN, 2018). In the latter report, the impact of breastfeeding on maternal health was also considered.
2. In 2019, SACN agreed to conduct a risk assessment on nutrition and maternal health focusing on maternal outcomes during pregnancy, childbirth, and up to 24 months after delivery; this would include the effects of chemical contaminants and excess nutrients in the diet.
3. SACN agreed that, where appropriate, other expert Committees would be consulted and asked to complete relevant risk assessments e.g., in the area of food safety advice. This subject was initially discussed during the horizon scanning item at the January 2020 meeting with a scoping paper being presented to the Committee in July 2020. This included background information on a provisional list of chemicals proposed by SACN. It was noted that the provisional list of chemicals was subject to change following discussion by the Committee on Toxicity of Chemicals in Food, Consumer Products, and the Environment (COT) which would be guiding the toxicological risk assessment process: candidate chemicals or chemical classes can be added or removed as the COT considered appropriate. The list was brought back to the COT with additional information in September 2020. Following discussion at the meeting, it was agreed that papers on several components should be prioritised and to this end, papers on iodine, vitamin D, and dietary supplements have been or will be presented to the Committee. The remaining list of compounds was to be triaged based on toxicity and exposure.
4. Following the discussion of the first prioritisation paper on substances to be considered for risk assessment by the COT, the Committee decided that each of the heavy metals (lead, mercury, cadmium, and arsenic) should be considered in separate papers.
5. A discussion paper (TOX-2023-20) was presented to the Committee at the March 2023 meeting, providing information on the toxicokinetics, toxicity, benchmark dose modelling and estimated exposures for total arsenic (tAs) and inorganic arsenic (iAs). The Committee highlighted that more detail was required regarding the potential epigenetic effects of arsenic (As) and that the aggregate exposure assessment required refinement to provide clarification of exposure estimates for the average dietary consumer alongside the values for high end consumption.
6. Following review of TOX-2023-20, the COT requested additional information on the epigenetic effects caused by arsenic (As) exposure. This paper is the additional literature review as requested by the Committee. A summary of the information presented in this paper has been included in the first draft statement on As in the maternal diet.
Background
7. Arsenic is described as a bright, silvery-grey group 15 metal, with an atomic number of 33 and a relative atomic mass of 75. Arsenic is used as a rodent poison and insecticide, a feed additive to prevent disease and improve weight gain in poultry, and in engineering, e.g. as a doping agent in semiconductors such as gallium arsenide (The Royal Society of Chemistry, 2023). Arsenic occurs in the environment in a variety of forms as a result of both natural and anthropogenic activity.
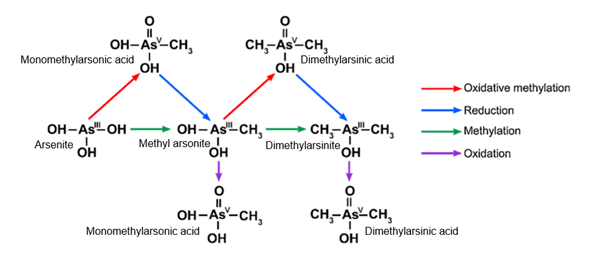
8. Acute exposure to iAs results in clinically symptoms such as nausea, vomiting, colicky abdominal pain, and diarrhoea with chronic iAs exposure resulting in symptoms such as multisystem disease and malignancy (Ratnaike, 2003). Arsenic and associated compounds have been considered by the International Agency for Research (IARC), with the most recent evaluation concluding that As and iAs compounds are carcinogenic to humans (Group 1) with sufficient evidence for carcinogenicity in particular for kidney, liver, and prostate (IARC, 2018). For organic As compounds, toxicity has shown to present to a lesser degree than iAs were generally, the lower the oxidation state of the compound the higher the toxicity (Luvonga et al., 2020).
Epigenetic Effects
9. The following paragraphs summarise the data found in the literature regarding the general epigenetic changes following As exposure and the changes following As exposure during gestation.
10. Epigenetic effects are changes in the expression of genes that don’t involve alteration of underlying Deoxyribose Nucleic Acid (DNA) sequences. Epigenetic changes can be inherited but can also be caused by external variables such as the environment and lifestyle. Changes in DNA methylation, histone modification and non-coding Ribonucleic Acid (RNA) regulation can alter an individual’s susceptibility to disease (Centre for Disease Control and Prevention, 2022).
11. The paper reviews the different types of epigenetic effects, then considers maternal-foetal effects, followed by carcinogenic effects and other longer term adverse outcomes arising from maternal exposure.
DNA Methylation
12. A review by Chakraborty et al. (2022) explored the epigenetic modifications and possible mechanisms for reprogramming that result from As exposure. The studies reviewed by the authors showed that microRNAs, DNA methylation, and histone modifications both in vivo and in vitro are the primary regulatory pathways that are affected by As exposure. The effects of As on DNA methylation showed that epigenetic changes can strongly influence DNA methyltransferase (DNMT) activity (Khan et al., 2017; Rea et al., 2017; Du et al., 2018). In environments oversaturated with As, S-adenosylmethionine (SAM) and S-adenosylhomocysteine (SAH) become depleted due to the increased rate of transfer of the methyl group from SAM onto the C-5′ position of cytosine at CpG dinucleotides to produce 5-methylcytosine. This reaction is catalysed by DNMT and when this is overstimulated and drains SAM stores, limitations in the availability of cofactors may affect subsequent DNMT activity.
13. In a study investigating As exposure and its association with genome-wide DNA methylation, links were found between CpGs and changes in As concentrations in whole blood which were shown to modulate As toxicity (Demanelis et al., 2019). A study conducted in women originating from the Andean region of Argentina with efficient As metabolism showed that with increasing As exposure, gene expression and hypermethylation was decreased in peripheral blood cells and expression of genes and six individual CpG sites increased. The genes identified were found to be associated with cancer and cell death. The age range and health status of study participants was unknown (Ameer et al., 2017).
14. Islam et al. (2022) reviewed several studies investigating DNA methylation, histone post-translational modification and RNA modification. The review summarises a study by Demanelis et al. (2019) which found that 34 CpGs were associated with urinary As concentration following exposure from tAs in drinking water in the Health Effects of Arsenic Longitudinal Study (HEALS) from Bangladesh (N= 396 adults). Results also showed a positive relationship between increasing As concentration and DNA hypomethylation in the CpGs identified. Most of the genes identified in the study were associated with reactive oxygen species (ROS) pathways, tumour necrosis factor alpha (TNF-α) signalling and inflammatory responses via nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB).
15. The review by Islam et al. (2022) also considered alternative splicing. A study by S. Liu et al. (2015, abstract only) found arsenite exposure caused direct binding of the As compound to the zinc fingers of Tet proteins. This binding weakened the catalytic efficiency of the Tet proteins converting 5-methylcytosine to 5-hydroxymethylcytosine, 5-formylcytosine, and 5-carboxylcytosine via oxidation. A dose-dependent increase was also seen in the levels of 5-hydroxymethylcytosine in DNA taken from human embryonic kidney (HEK) 293T cells which overexpressed the catalytic domain.
16. A study by Rager et al. (2017, abstract only) investigated the concentration of iAs that would elicit transcriptomic, proteomic, epigenomic, and integrated multi-omic changes in cord blood using benchmark dose modelling. Varying levels of total urinary As concentrations were modelled against various endpoints in cord blood including genome-wide DNA methylation, microRNA expression, mRNA expression, and protein expression levels. DNA methylation was observed to be affected at lower As concentrations compared to other endpoints. One eigengene (which has been defined as ‘the first right-singular vector of the standardized module expression data’ (Langfelder and Horvath, 2007)) was linked to reduced gestational age with increasing iAs exposure. ‘Genes/proteins within this module eigengene showed enrichment for organismal development, including potassium voltage-gated channel subfamily Q member 1 (KCNQ1), an imprinted gene showing differential methylation and expression in response to iAs’. The benchmark dose level (BMD(L)) modelled from the prioritized multi-omic module eigengene was calculated as 58(45) µg/L urinary tAs from an estimated concentration of 51(40) µg/L iAs in drinking water. (Details of the BMD(L) will be further clarified when the full paper becomes available).
17. In a cohort study with 40 women from Northern Chile, participants with high and low As exposures (555 µg/L and 2 µg/L respectively in drinking water) were selected and DNA methylation was measured in their peripheral blood mononuclear cells (PBMC) and buccal cells. The study found that those participants that had been exposed to high levels of As had an accelerated ‘PhenoAge’ (a new epigenetic biomarker of aging) (Levine et al., 2018) of six years, demonstrated by a positive correlation with DNA methylation aging biomarkers and negative correlation with DNA telomere length in PBMCs, when compared to participants exposed to low As levels. However, analysis of buccal cells showed no significant association. Cell-type composition adjustments revealed that there were positive associations between Hannum-based epigenetic age acceleration (Hannum EAA), skin and blood EAA and extrinsic EAA, suggesting that early life exposure to As may be associated with accelerated biological ageing (Bozack et al., 2022).
Histone Modifications
18. Chakraborty et al., (2022) further described how As caused a large disruption in histone post translational modifications which has the ability to induce structural perturbations, resulting in chromosomal instability and from this, induce carcinogenesis (Martinez-Zamudio and Ha, 2011). Methyltransferases, demethylases, acetyl transferases, deiminases and kinases have all shown direct interaction with arsenicals and result in different post translational modifications of histones depending on the enzyme targeted (Bannister and Kouzarides, 2011).
19. Phosphorylation of histones has proven to be affected by chronic As exposure in several ways, with an ultimate endpoint of DNA damage by interfering with chromosome condensation during the cell cycle (Prigent and Dimitrov, 2003; Rossetto, Avvakumov and Côté, 2012). Dose-dependent phosphorylation has been seen in H3S10 (Histone H3 serine 10) histones (Li et al., 2002; Suzuki, Kita and Ochi, 2013; Ray, Huang and Tsuji, 2015, p. 2) following exposure to arsenite. Cobo, Valdez and Gurley, (1995) found that an elevated number of malignancies resulting from induced chromosomal damage due to a decrease in H1 and H3 phosphorylation following arsenite exposure (10 µM) in Chinese hamster cells. Furthermore, chronic As exposure affects enzymes involved in the acetylation process of histones. In particular, CASPASE-10 expression has increased following exposure to As and in turn has been linked to As induced apoptosis (Li et al., 2002).
20. Islam et al. (2022) reviewed papers discussing histone modifications following exposure to As and subsequent oxidative damage (Ma et al. (2016, abstract only)) The study included 138 individuals from Guizhou province, China exposed to high levels of As due to exposure from cooking with coal (urinary concentration 37.43 µg/g and hair concentration 0.27 µg/g) and 77 individuals at low levels of exposure (the control group) (urinary concentration 15.61 µg/g and hair concentration 0.13 µg/g). Urinary and hair concentrations of As were correlated with altered global levels of histone 3 lysine 18 acetylation (H3K18ac), histone H3 lysine 9 dimethylation (H3K9me2), and histone 3 lysine 36 trimethylation (H3K36me3) in human peripheral lymphocytes. Modifications of H3K18ac and H3K36me3 were enhanced in the gene promotors linked to
21. Suzuki et al., (2009) demonstrated that along with As itself, As metabolites including dimethylarsinite (DMA(III)) have the potential to cause spindle formation abnormalities, preventing cytokinesis. This results in failures in cell division, creating multinucleated cells and hence can instigate tumorigenesis. Several other studies also concluded that As exposure can affect the cell cycle at prometaphase, interphase (Prigent and Dimitrov, 2003; Suzuki et al., 2009) and during transcriptional initiation (Lo et al., 2000; Zhang, 2003).
microRNA Modifications
22. Micro RNAs are small, highly conserved non-coding RNA molecules which are involved in the regulation of gene expression. Several studies have showed that As exposure can dysregulate many microRNAs (miRNAs) in vitro (Michailidi et al., 2015; Liu et al., 2016; Banerjee et al., 2017) with miR-21 and miR-199a strongly liked with lung damage following exposure to As (Luo et al., 2015; He et al., 2019). Arsenic has been shown to alter the pattern of miRNA expression by upregulating miR-21, miR-141, miR-200a, (in non-malignant human keratinocyte (HaCat) cells) which have all shown to be involved in carcinogenesis (Gonzalez et al., 2015). Upregulation of miR-155 was also seen in human bronchial epithelial (HBE) cells following As exposure (sodium arsenite) for 13 weeks at 2.5 µM (Chen et al., 2017).
23. Population based studies showed links between miRNAs, As exposure and multiorgan damage (Zeng et al., 2019). Several miRNAs were associated with damage to multiple organs including an association of miR-191 with kidney damage, miR-155 with greater risk of skin manifestation effects and miR-21 and miR-145 with damage to the liver. Another population study by Banerjee et al. (2019) investigated the changes in miRNA expression on skin lesions. Populations exposed to As in this study showed overexpression of miR-21, miR-23a, miR-27a, miR-122, miR-124, miR-126, miR-619, and miR-3613 and downregulation of miR-1282 and miR-4350. These miRNAs were shown to target distinct biological pathways and hence elicit different biological responses.
24. The review by Chakraborty et al., (2022) also highlighted changes in miRNA expression following prenatal As exposure. Rager et al., (2014) observed that differential expression of several miRNAs in newborn cord blood was associated with an increased maternal urinary As levels. Pathway analysis of the differentially expressed miRNAs showed that over expressions were associated with pathways that led to adverse outcomes including cancer and type 2 diabetes (T2D). miRNAs with decreased expression were linked to the silencing of key genes associated with immune response and hence may affect the innate and adaptive immune response in infants.
25. In a study by Zeng et al., (2019, abstract only), miR-21 upregulation was associated with arsenic-induced skin damage, while miR-191 upregulation was associated with kidney damage. This study suggested that arsenic-induced organ damage was associated with changes in specific miRNA levels.
Maternal/ Foetal Effects
Human Studies
26. Smeester et al. (2017) considered the connection between the concentrations of toxic metals, including As, in amniotic fluid and fetal gene expression in a cohort study with 42 participants. The species of As were not stated in the study. The concentration of As in amniotic fluid was reported as 3.4 to 41.3 µg/L with a mean concentration of 16.3 µg/L. Multivariable models found that greater As levels in amniotic fluid were associated with increased expression levels of three gene types, i.e. olfactory receptor (OR4S2), phospholipase C (phosphoinositide-specific) (PLCB1), and progesterone receptor (PGR). All of these gene types have been associated with adverse birth outcomes and reproductive effects and are involved in the key pathways that may be related to spontaneous preterm birth. OR4S2 has previously been linked to an increased risk of preterm birth when increased copies of variants occurred (Biggio et al., 2015). Arsenic has been associated with upregulation of PLCB1, which plays an important role in extracellular signalling and can cause intrauterine growth restriction (Sitras et al., 2009). None of the metals evaluated by Smeester et al., (2017), including As, showed any association with adverse outcomes relating to gestational age.
27. Winterbottom et al. (2019) assessed the effects of increasing tAs exposure on the biological functions of the foetal placenta and consequently foetal health and development. The study analysed 46 infants from a cohort study undertaken in New Hampshire. Prenatal As exposure was assessed by collection of maternal urine samples between 24 - 28 weeks of gestation and birth gestational age (weeks) was estimated from ultrasound measurements collected at the time of enrolment. The analysis of urine also measured individual As species due to the high levels of tAs found in the samples and therefore tested for arsenite (As(III)), arsenate (As(V)), dimethylarsinic acid (DMA(V)), dimethylarsinic acid (DMAA(V)), methylarsonous acid (MMAA), and arsenobetaine (AB). However, AB was excluded from the analysis due to its perceived nontoxicity. RNA sequencing was used to analyse changes in gene expression by review of placental samples. Results showed sex-specific differences. In female placenta, results indicated that no genes were differentially expressed between high and low As exposure groups using a false discovery adjustment of <0.05. However, associations were found with LEM Domain Containing 1 (LEMD1) and Uroplakin 3B (UPK3B) with 2.51- and 2.48- fold changes in expression following higher tAs exposure. In male fetal placenta, 606 genes were expressed differentially between high and low As exposure with Fin Bud Initiation Factor Homolog (FIBIN) and RAN Binding Protein 3 Like (RANBP3L) having the greatest association with 0.14- and 0.15-fold changes respectively. Gene set enrichment analysis showed that 211 gene sets in the female placenta and 154 in the male placenta were enriched with differentially expressed genes following higher tAs exposure. In the female placenta, 103 of the gene sets were linked with lower weights at birth. The study found that overall, tAs could affect multiple biological mechanisms in the placenta and that a subset of gene expression effects is sex dependent.
28. Deyssenroth et al. (2022) used maternal toenail clippings from the Rhode Island Child Health Study (RICHS, N = 199) to measure tAs concentration and its effects on alterations of placental gene transcript proportions and associated birth weight differences. Placental samples were reviewed to determine placental transcriptome and single nucleotide polymorphisms. Infants that were small for their gestational age had 82 genes that were associated with differential transcript usage (DTU) where the gene ORMDL sphingolipid Biosynthesis regulator 1 (ORMDL1) showed DTU association with increased exposure to As. The authors concluded that these changes suggested that increased in utero exposure to tAs is associated with DTU and reduced fetal growth, potentially linked to disturbances in placental mechanisms.
29. Laine and Fry (2016) reviewed the effects of prenatal iAs exposure on perturbation of major genes and/or proteins and highlighted that prenatal iAs exposure results in several fetal epigenetic changes including CpG methylation, gene expression and protein expression. In total, 845 genes were key regulators associated with prenatal iAs exposure and iAs exposure was related to alteration of 61 genes linked to two molecular endpoints, 54 genes linked to altered levels of gene expression and CpG methylation and seven genes with altered gene and protein expression.
30. Martinez and Lam (2021) reviewed the adverse health effects linked to pre- and perinatal As exposure. Inorganic As can directly influence molecular pathways involved in disease progression by altering, e.g., genomic instability correlated with oxidative damage, global and localized epigenetic reprogramming, alteration of gene expression (including coding and non-coding RNAs), and histone post-translational modifications. At a genetic level, As exposure has been shown to promote oxidative and genotoxic damage by formation of ROS species (Kitchin and Conolly, 2010; Smeester et al., 2011; Minatel et al., 2018; Smeester and Fry, 2018).
31. Epigenetic effects and epigenetic reprogramme disease susceptibility have been demonstrated after long-term exposure to As by decreased SAM levels due to the competition from As methylation, thus diverting SAM from epigenetic processes that require methyl groups (Simeonova and Luster, 2000; Reichard and Puga, 2010; Ouyang et al., 2020). The depletion of methyl groups via this mechanism and inhibition of DNA methyltransferases by As can cause global hypomethylation and additionally, can lead to reduced methylation at specific regions of DNA and at gene promoters. Studies have shown that As promotes Septin-9 (SEPT9) in human colorectal cancer cell lines (Rafiei et al., 2019) and leads to hypomethylation of the Excision Repair 2, TFIIH Core Complex Helicase Subunit (ERCC2) promoter, in turn leading to increased ERCC2 expression and decreased p53 phosphorylation which could result in downstream DNA damage (serine 392) (Paul et al., 2014).
32. As has also been shown to affect methylation of mitochondrial DNA, influencing and increasing expression of nicotinamide adenine dinucleotide phosphate hydrogen dehydrogenase (ND) 4, ND6, mitochondrial transcription factor A (mtTfam) and higher mitochondrial DNA copy number (mtDNAcn) (Sanyal et al., 2018). Further damage to the mitochondria has been shown to result via the formation of ROS and subsequent oxidative damage, for example, through stimulation of epidermal growth factor receptor (EGFR) in the mitochondria which in turn dysregulated reserve cells, increased mitochondrial ROS, and in turn increasing proliferative signalling in Murine C2C12 myoblasts (Cheikhi et al., 2020). Disruption of EGFR can also affect differentiation in cell types from cyclin D1 dysregulation. The latter can occur at low level As exposure, however, at higher concentrations, additional detrimental effects have been demonstrated, including the inhibition of mitochondrial adenosine triphosphate (ATP) generation and ultimately cell death (Cheikhi et al., 2020).
33. Arsenic has been shown to decrease methylation in some DNA regions with non-coding sequences, particularly in long interspersed nuclear element-1 (LINE-1) among female individuals (Hossain et al., 2017) where LINE-1 hypomethylation has been linked to non-favourable cardiac health outcomes (Muka et al., 2016). Arsenic exposure during pregnancy has been linked to hypomethylation of cytosines, causing ‘accumulation in the promoter regions of the active full-length L1MdA subfamily of LINEs, potentially enhancing retro transposition and cryptic promoter activity of 5' long-terminal repeats for coding genes and non-coding RNAs (Nohara et al., 2020).
34. Dose-dependent relationships have also been demonstrated between in utero As exposure and methylation at individual CpG loci in white cord blood cells (Vaiserman and Lushchak, 2021). Leukocytes in both mother and foetus were positively associated with LINE-1 methylation levels following high levels of exposure (1.9–230 μg/L) to As in drinking water. An association was also found with methylation of CpG sites in p16, a tumour suppressor gene, but to a lesser extent (Kile et al., 2012).
35. In a study investigating the cord blood cells from 21 newborns exposed to As in utero (control n = 11 unexposed infants) (unexposed maternal toenail <0.5 μg/g or exposed maternal toenail ≥0.5 μg/g) microarray analysis identified 450 differentially expressed genes relating to inflammation, apoptosis, and activation of molecular stress pathways. An association was identified between maternal As concentration in blood and soluble fms-like tyrosine kinase-1 (sFLT1) gene expression, linking As exposure with reduced placental angiogenesis, slowing foetal growth (Fry et al., 2007). Exposure to As has further been linked to changes in DNA methylation in p53 promoter regions in cord blood lymphocytes, which has been suggested as a mechanistic link between As exposure and carcinogenesis (Intarasunanont et al., 2012) see below for discussion of this topic.
36. Rojas et al., (2015) demonstrated that arsenic exposure was associated with changes in methylation patterns and mRNA patterns that were enriched for binding sites of CCCTC-binding factor transcription factors and early growth response in newborn cord blood lymphocytes. Methylation patterns in seven of these genes were associated with gestational age and head circumference, suggesting a link between arsenic exposure, DNA methylation, and adverse birth outcomes.
37. Bozack et al. (2018) examined mothers exposed to As via drinking water (determined through measurement of maternal toenails) < 1month post-partum from a cohort in Bangladesh. DNA methylation was measured in cord blood and the results showed that As exposure was associated with differential DNA methylation of 139 different loci linked to gestational age. Doubling the As exposure was associated with a reduction in gestational age of 2 days (the basis of the comparison for the finding on gestational age is unclear). This effect was shown to be mediated fully by the principal component of the top-ten CpGs, whilst miRN214-3 and MCC DNA methylation were shown to both directly and indirectly affect gestational age. Overall, the study found that prenatal exposure to As lowered DNA methylation of miR124-3, mediating a reduction in gestational age.
38. A review by Bermick and Schaller, (2022) showed that As exposure in utero can lead to differential DNA methylation in umbilical cord blood and poor cognitive function. Arsenic was shown to increase expression of immunomodulatory micro-RNAs. In umbilical cord blood, let-7a, miR-126, miR-16, miR-17, miR-20a, miR-20b, miR-96, and miR-98 are seen to be affected. Differentially methylated sites were also affected by As exposure where the sites were found to map pathways involved in natural killer cell cytotoxicity, leukocyte migrations, transforming growth factor (TGF)- β signalling, and antigen processing and presentation.
39. In a cohort study by Winterbottom, Moroishi, et al. (2019) analysing 138 genes including reader, writer and eraser genes of post-translational histone modifications (PTHM), that encode primary epigenetic regulators in the placenta, results showed that expression levels of 27 of the 138 genes tested were linked to parental As exposure. When analysed by sex, As exposure was linked to 40 genes in the male placenta and 3 non-overlapping genes in the female placenta. The expression of the putative histone-lysine N-methyltransferase (PRDM6) gene encoding for histone methyltransferase appears to have an inverse relationship to As exposure. Mutations in this gene have previously been associated with patent ductus arteriosus, a congenital heart defect.
40. Bozack et al. (2020) examined the mediation of adverse birth outcomes by DNA methylation levels of three DNMT3A CpGs in cord blood following in utero As exposure from a cohort of 413 newborns of exposed mothers in Bangladesh. Exposure to As via drinking water was measured from maternal toenails and changes in DNMT3A were measured in foetal cord blood. Results showed that DNMT3A DNA methylation was associated with gestational age (B = −0.10 weeks) and birth weight (B = −11.0 g). Overall, a 2-fold increase in maternal toenail concentration was associated with a decrease in birthweight (29 grams) and a decrease in gestational age by 2.1 days.
41. Overall, exposures to As in utero have been associated with a number of adverse outcomes, linking changes in DNA methylation in the placenta and cord blood in both a time and sex-dependent manner. DNA methylation in cord blood has shown to be greater in male infants compared to female infants following maternal exposure while As exposure during later trimesters of pregnancy has shown a weaker association with cord blood DNA methylation compared exposures during early stages of pregnancy (Vaiserman and Lushchak, 2021). Conversely, some studies have shown evidence of reduced methylation while others support hypermethylation after As exposure. However, as a whole, exposure to As has shown to alter epigenetic modifications and hence perturbate As related disease pathways.
Animal Studies
42. In utero exposure in animal studies found similar associations between As exposure and hypomethylation as have been demonstrated in humans. A study by Waalkes et al. (2004) conducted using adult male mice (offspring of exposed mothers) showed that hypomethylation of genes involved in oestrogen signalling paralleled an increase in mRNA expression seen in hepatic tumours of mice exposed to As in utero.
Prenatal As exposure (5 rats born to mothers supplied drinking water containing 0 ppm As and eight of the adult male mice born to mothers supplied drinking water containing 85 ppm arsenic from gestation day 8 through day 18) was associated with adverse effects linked to histone modification. An increase in genome-wide hypo-acetylation at H3K9 and H3K4 trimethylation in the promoter region of fatty acid binding protein 4 (Fabp4) was observed in exposed mice at a concentration of 85 ppm in drinking water (Nohara et al., 2012) along with an increase in miRNA-21 expression. miRNA-21 is particularly known for its role in carcinogenesis, (Liu et al., 2020). Apoptosis and cell proliferation/migration has also been documented after As exposure influenced by disrupted expression of the miR-143 (exposure at 5 µM iAs in human prostate stem cells) and miR-27a (exposure at in HBE cells) miRNAs respectively (Ngalame et al., 2016; Zhang et al., 2016).
Carcinogenesis
43. Arsenic is a well-known carcinogen, however, the molecular mechanism by which As induces cancer has not yet been fully described. Arsenic is non-mutagenic and has been shown to induce carcinogenesis via epigenetic-regulated gene expression alterations. Two carcinogenic pathways have been suggested, modification of the epigenome via direct interaction with chromatin remodelers and indirectly through generation of ROS that interfere with chromatin remodelers (George et al., 2023). (Chromosome remodelling is an enzyme mediated process by which the condensed chromatic is made accessible to the cell’s transcription machinery).
44. One of the main mechanisms proposed for As induced carcinogenicity is a type of RNA epigenetic modification called N6-methyladenosine (m6A). A study by Zhao et al. (2023) demonstrated that arsenic exposure increased m6A modification of genes regulating ribosome biogenesis, which leads to a post-transcriptional upregulation of ribosome biogenesis. This upregulation in turn stabilised ribosomal proteins and modulated non-coding RNA molecules that target ribosomal RNAs and proteins. This series of events ultimately leads to skin cancer. The authors suggested that a recognized proliferation signalling node, Ak strain transforming (AT) K1, was a mediator in this carcinogenesis process. Yang and Zhang (2022), (abstract only) also investigated the role of m6A RNA modification and its role in inflammatory homeostasis of skin lesions following As exposure. In human keratocytes, As exposure led to irregular expression of m6A RNA methylation regulators and cytokines. This upregulation of RNA methyltransferase-like-3 (METTL3) increased levels of m6A, subsequently leading to disturbed secretion of multiple inflammatory homeostatic indicators including IL-6, IL-17, and IL-10. In human skin samples exposed to As, upregulated METTL3 further elevated keratins (Krt), Krt1 and Krt10 levels which are known biomarkers of As-induced skin lesions. The authors concluded that METTL3 was associated with inflammatory homeostasis and skin lesions in exposed individuals and upregulation of this gene increased successive effects on cytokines and keratins. In HaCat cells, knocking down or upregulating METTL3 antagonised and facilitated arsenite-induced imbalances in inflammatory homeostasis and keratinocyte damage respectively.
45. Genes differentially linked to CpG methylation showed enrichment of the Myc-mediated apoptosis pathway as well as G1/S checkpoint regulation and tumour protein p53 pathways (Laine and Fry, 2016). Altered gene expressions resulting from iAs exposures was linked to inflammatory and immune response pathways; (toll-like receptor (TLR), glucocorticoid receptor, inducible nitric oxide synthase (iNOS), and IL-6 and altered protein expression genes showed enrichment for growth factors involved in inflammatory pathways (TGF-β, bone morphogenetic protein (BMP) signalling pathway, and fibroblast growth factors).
46. Genchi et al. (2022) reviewed the epigenetic effects of As exposure and its links with carcinogenicity. Arsenic, in the form of methylarsonous acid (MMA(III)) and As(III), was shown to reduce histone 4 lysine 16 (H4K16) acetylation in human bladder cells (Jo et al., 2009) and As(III) also increased H3K9 demethylation (H3K9me2) and decreased H3K27 trimethylation (H3K27me3) in lung carcinoma cells (Zhou et al., 2008, 2009).
47. Arsenic has been shown to alter expression of several miRNAs in human bladder and liver cells, where the latter showed upregulation of miR-24, miR-29a, miR-30a, and miR-210, where miR-29a had a positive effect on cancer formation by inducing apoptosis and inhibited cell growth (Meng et al., 2011). The review by Genchi et al. (2022) also highlighted the effects of As exposure (as iAs, MMA(III) and DMA(III)) on arsenic methyltransferase (AS3MT) and miRNA expression and found that exposure was negatively correlated with AS3MT expression and miR-548c-3p, both of which both regulate As methylation (Cheng et al., 2018). Arsenic was also involved in the reduction of DNMT activity and the changes in the availability of SAM in CpG methylation. Arsenic is known to affect gene silencing by CpG methylation which can directly affect the binding affinity of a number of transcription factors to their regions of DNA. CpG islands were also affected by As, with a study by Koestler et al. (2013) demonstrating that in utero exposure could cause cancer and congenital malfunctions. DNA methylation of cord blood derived DNA was measured in a cohort of 134 exposed infants with further measurement of methylation to individual CpG loci. Of 44 CpG island identified, three quarters of the islands showed greater methylation following higher exposures to As.
48. The carcinogenicity of As and its mechanism of action (MoA), specifically in women (tumorigenic action in embryonic kidney HEK239T and cervix-carcinoma HELA human cells was reviewed by Olmedo-Suárez et al. (2022). The authors found that As decreased acetylation of H4K16 in a dose dependent manner. The authors further noted that exposure to As reduced histone acetyltransferase (HAT) through binding directly with cysteine into the Cys2HisCys zinc finger domain (Liu et al., 2015). Pournara et al. (2016) showed, through analysis of CD4+ cells, that women with higher exposure to As (as measured by higher urinary As concentrations) had significantly reduced levels of global trimethylated Lys-9 of histone H3 (H3K9me3). This suggested that when histone methylation was decreased, expression of genes involved in tumorigenesis were triggered. Furthermore, in BEAS-2B and human lung cancer tissues, upregulation of the miRNA, miR-301a by the IL6/STAT3/ mothers against decapentaplegic homolog 4 (SMAD4) signalling pathway was observed, this pathway has been demonstrated to contribute to the causation of cancer (Pournara et al., 2016).
49. Mechanistic studies reviewing the effects of As on cancerous pathways have also assessed the role of miRNAs. Luo et al. (2013) suggested that As exposure induced secretion of interleukin (IL) 6, mediated the signalling of signal transducer and activator of transcription 3 (STAT3) which in turn upregulated miR-21, increasing epithelial mesenchymal transition, indicating a potential mechanism for lung cancer formation. Zhong et al., (2018) also found overexpression of miR-301 following As exposure in human bronchial epithelial cell lines (BEAs) 2B through IL-6/STAT3 signalling.
50. Exposure to As has also been suggested to induce epigenetic changes by generation of As-induced oxidative stress (He et al., 2014; Guo et al., 2020). As-induced ROS have been suggested to promote tumour growth and angiogenesis (He et al., 2014). and a study by Ling et al. (2012) showed that miR-21 upregulation was involved in malignant changes in human embryo lung fibroblast cells which, following As exposure, was mediated by ROS-mediated activation of the extracellular signal-regulated kinase (ERK)/ NF-κB pathway.
51. Several studies have concluded that As exposure can downregulate miRNAs (Wang et al., 2014; Michailidi et al., 2015; Ngalame et al., 2016; Liu and Bain, 2018) including miR-200b, an inhibitor of cancer metastasis and tumour suppressor (Wang et al., 2011; Michailidi et al., 2015). Other studies found that As can downregulate miR-31 leading to malignant cell formation (Chen et al., 2018) and overexpression of miR-143 expression resulting in increased cell proliferation and apoptotic resistance (Ngalame et al., 2016).
Other Effects
52. T2D was shown to be one of the most frequent, non-cancerous health disorders associated with As exposure (Grau-Pérez et al., 2017; Eick et al., 2019; Dai et al., 2020) with epigenomic changes being observed among exposed individuals (Maull et al., 2012). miR-NA-146a has been linked with iAs induced T2D, potentially by decreasing insulin secretion through decreased expression of calcium dependent protein kinase (CamK2a) (Beck et al., 2019).
53. Small ubiquitin like modifier (SUMo) moieties and changes in SUMoylation patterns have been linked to DNA methylation and other epigenetic changes as a result of As exposure. Arsenic exposure aids the overexpression of SUMoylated histones and was also associated with SUMoylation of Mus81 DNA endonuclease, which is important for chromosome congression (where the chromosomes align on the spindle equator) during mitosis and thus a factor in the mediation of chromosomal alignment (Hu et al., 2017).
54. Domingo-Relloso et al. (2022) analysed blood DNA methylation in 2,321 participants (mean age 56.2, 58.6% women) from the Strong Heart Study of American Indian origin following exposure to As, measured by urinary analysis. Differentially methylated positions (DMP) were identified by the authors as potential mediators between cardiovascular disease and As exposure. The authors identified a total of 20 and 13 DMPs as mediators for cardiovascular disease incidence and mortality respectively. Several of the genes identified were found to be further linked to diabetes.
55. In a review by Laine and Fry (2016), seven genes were common across the 12 studies evaluated and these genes were associated with enrichment of pathways regulated by tumour necrosis factor (TNF). TNF has been shown to play a vital role in developmental-related signalling, cellular growth signalling and inflammation. TNF has also been associated with As related diseases where polymorphisms within the TNF promoter have increased the levels of TNF and subsequently increased the incidence of conjunctivitis, respiratory disease, and skin lesions. The authors concluded that “TNF may be an important signalling molecule mediating the relationship between prenatal iAs exposure and iAs-associated disease” (Laine and Fry, 2016).
56. Arsenic has also been linked to endocrine disruption through epigenetic influence following gestational exposure. Gangopadhyay et al. (2019, abstract only) noted that biphasic responses from high and low As exposures on epigenome remodelling were particularly prominent during exposure in the early stages of life. Arsenic exposure during foetal development has been shown to alter the functional epigenome of the foetus by altering DNA methylation patterns, histone modifications and changes in miRNA in a tissue-specific manner. Reproductive effects have been demonstrated by disruption of the endocrine system in newborns through epigenetic changes in hormonal imprinting and through irreversible modulation (Gangopadhyay et al., 2019).
57. In a study by Kaushal et al. (2017), the maternal urinary As exposure of 64 mother infant pairs (in utero exposure) from Taiwan were selected to undergo DNA methylation analysis. Arsenic exposure was determined through measurement of iAs, its metabolites and the sum of these (tAs) in maternal urine. It was found that approximately 579 CpGs had differential methylation levels associated with arsenic exposure, and their functional annotation indicated pathways for cardiovascular disease and T2D. It was also demonstrated that methylation levels of 5 CpGs (cg25189764, cg04986899, cg04903360, cg08198265 and cg10473311) was associated positively with low density lipoprotein, a biomarker for cardiovascular disease and diabetes in later life, over time.
58. The review by Martinez and Lam (2021) also discussed epigenetic effects caused by As during pregnancy and noted a positive correlation between DNA hypomethylation in cord blood and As concentration in maternal urine (Pilsner et al., 2012). However, in utero exposure has also been linked to DNA hypermethylation in the promoting region of extracellular matrix remodelling gene matrix metalloproteinase 9 (MMP9) with parallel reductions in MMP9 protein levels (Chicoine et al., 2002; Gonzalez-Cortes et al., 2017). In addition, in utero exposure has caused sequence changes in umbilical cord leukocytes, increasing methylation in repetitive sequences and in promoter regions of some genes linked with tumour suppression, including cyclin dependent kinase inhibitor 2A (CDKN2A) and transformation-related protein 53 (TP53) (Kile et al., 2012; Cardenas et al., 2015).
Summary
59. Evidence has shown that exposure to As can cause epigenetic changes by different modes of action including DNA methylation, histone modification and microRNA modification. These effects can manifest in the general population at a cellular level causing apoptosis and hinderance of cell division along with inflammatory responses, organ damage and carcinogenesis.
60. In terms of maternal health, As exposure affected genes linked to preterm birth and reduced foetal growth. Sex-specific differences were also seen following high tAs exposure where 211 and 154 genes in female and male respectively were enriched with differentially expressed genes. In utero exposure to As showed to increase expression of genes linked to adverse birth outcomes, upregulate genes involved in extracellular signalling and intrauterine growth restriction, decrease SAM and inhibit DNA methyltransferases.
Questions to the Committee
1. Does the Committee have any comments on the potential effects of arsenic on maternal or fetal health?
2. Does the Committee have any other comments on the contents of this review?
3. Which information should be included in the statement?
Secretariat
October 2023
Abbreviations
Table 10: List of abbreviations and their full meanings.
|
Abbreviation |
Meaning |
|
AB |
Arsenobetaine |
|
As |
Arsenic |
|
As(III) |
Arsenite |
|
As(V) |
Arsenate |
|
AS3MT |
Arsenic methyltransferase |
|
ATK |
Ak strain transforming |
|
ATP |
Adenosine triphosphate |
|
BEAS |
Human bronchial epithelial cell lines |
|
BMDL |
Benchmark dose level |
|
CamK2a |
Calcium dependent protein kinase |
|
COT |
Committee on Toxicity |
|
CDKN2A |
Cyclin dependent kinase inhibitor 2A |
|
DMA(III) |
Dimethylarsinite |
|
DMA(V) |
Dimethylarsinate |
|
DMAA(V) |
Dimethylarsinic acid |
|
DMP |
Differentially methylated position |
|
DNA |
Deoxyribose Nucleic Acid |
|
DNMT |
DNA methyltransferase |
|
DTU |
Differential transcript usage |
|
EGFR |
Epidermal growth factor receptor |
|
ERCC2 |
Excision Repair 2, TFIIH Core Complex Helicase Subunit |
|
ERK |
Extracellular signal-regulated kinase |
|
Fabq4 |
Fatty acid binding protein 4 |
|
FIBIN |
Fin Bud Initiation Factor Homolog |
|
H3K18ac |
Histone 3 lysine 18 acetylation |
|
H3K27me3 |
H3K27 trimethylation |
|
H3K36me3 |
Histone 3 lysine 36 trimethylation |
|
H3K9me2 |
Histone H3 lysine 9 dimethylation |
|
H3K9me3 |
Trimethylated Lys-9 of histone H3 |
|
H3S10 |
Histone H3 Serine 10 |
|
H4K16 |
Lysine 16 of histone |
|
HaCat |
Human keratinocyte |
|
HAT |
Histone acetyltransferase |
|
HBE |
Human bronchial epithelial |
|
HEALS |
Health Effects of Arsenic Longitudinal Study |
|
HEK |
Human embryonic kidney |
|
Hannum EAA |
Hamun-based epigenetic age acceleration |
|
IARC |
International Agency for Research |
|
iAs |
Inorganic Arsenic |
|
IL |
Interleukin |
|
iNOS |
Induced nitric oxide synthase |
|
LEMD1 |
LEM Domain Containing 1 |
|
LINE-1 |
Long interspersed nuclear element |
|
KCNQ1 |
Potassium voltage-gated channel subfamily Q member 1 |
|
Krt |
Keratin |
|
m6A |
N6-methyladenosine |
|
METTL3 |
Methyltransferase-like-3 |
|
miRNA |
microRNA |
|
MMA(III) |
Methylarsonous acid |
|
MMAA |
Methylarsonous acid |
|
MMP |
Matrix metalloproteinase 9 |
|
MoA |
Mechanism of aciton |
|
mtDNAcn |
Mitochondrial DNA copy number |
|
mtTfam |
Mitochondrial transcription factor A |
|
ND |
nicotinamide adenine dinucleotide phosphate hydrogen dehydrogenase |
|
NF-κB |
Nuclear factor kappa-light-chain-enhancer of activated B cells |
|
OR4S2 |
Olfactory Receptor, Family 4, Subfamily S, Member 2 |
|
ORMDL1 |
ORMDL Sphingolipid Biosynthesis Regulator 1 |
|
P4 |
Progesterone |
|
PGR |
Progesterone Receptor |
|
PLCB1 |
Phospholipase C, Beta 1 |
|
PRDM6 |
Putative histone-lysine N-methyltransferase |
|
PTHM |
Post translational histone modifications |
|
RANBP3L |
RAN Binding Protein 3 Like |
|
RICHS |
Rhode Island Child Health Study |
|
RNA |
Ribonucleic acid |
|
ROS |
Reactive Oxygen Species |
|
SACN |
The Scientific Advisory Committee on Nutrition |
|
SAH |
S-adenosylhomocysteine |
|
SAM |
S-adenosylmethionine |
|
SEPT9 |
Septin-9 |
|
sFLT1 |
Soluble fms-like tyrosine kinase-1 |
|
SMAD4 |
Mothers against decapentaplegic homolog 4 |
|
STAT3 |
Signal transducer and activator of transcription 3 |
|
SUMo |
Small Ubiquitin like Modifier |
|
tAs |
Total Arsenic |
|
T2D |
Type-2 Diabetes |
|
TGF |
Transforming growth factor |
|
TLR |
Toll-like receptor |
|
TNF |
Tumour necrosis factor |
|
TP53 |
Transformation-related protein 53 |
|
UPK3B |
Uroplakin 3B |
|
PBMC |
Peripheral blood mononuclear cells |
Search Terms
The references cited in this discussion paper are of publications found in Ebsco, Pubmed, Scopus and Springer, searched using Lit fetch. The publications retrieved were selected using the following search terms:
|
Arsenic, Arsenolipids, Arsenosugars, Arsenobetaine, Arsenocholine, Organoarsenic. |
And
|
Pregnancy, Preconception, Lactation, Fertility, Pregnancy Chances, Birth Outcomes, Absorption, Distribution, Metabolism. |
For Epigenetic Literature Review:
|
Arsenic
|
And
|
Epigenetic
|
References
Ameer, S.S. et al. (2017) ‘Arsenic exposure from drinking water is associated with decreased gene expression and increased DNA methylation in peripheral blood’, Toxicology and Applied Pharmacology, 321, pp. 57–66: https://doi.org/10.1016/j.taap.2017.02.019
Banerjee, N. et al. (2017) ‘Increased microRNA 21 expression contributes to arsenic induced skin lesions, skin cancers and respiratory distress in chronically exposed individuals’, Toxicology, 378, pp. 10–16: https://doi.org/10.1016/j.tox.2017.01.006
Banerjee, N. et al. (2019) ‘MicroRNAs play an important role in contributing to arsenic susceptibility in the chronically exposed individuals of West Bengal, India’, Environmental Science and Pollution Research, 26(27), pp. 28052–28061: https://doi.org/10.1007/s11356-019-05980-8
Bannister, A.J. and Kouzarides, T. (2011) ‘Regulation of chromatin by histone modifications’, Cell Research, 21(3), pp. 381–395: Regulation of chromatin by histone modifications | Cell Research (nature.com)
Beck, R. et al. (2019) ‘Arsenic is more potent than cadmium or manganese in disrupting the INS-1 beta cell microRNA landscape’, Archives of Toxicology, 93(11), pp. 3099–3109: Arsenic is more potent than cadmium or manganese in disrupting the INS-1 beta cell microRNA landscape | SpringerLink
Bermick, J. and Schaller, M. (2022) ‘Epigenetic regulation of pediatric and neonatal immune responses’, Pediatric Research, 91(2), pp. 297–327: Epigenetic regulation of pediatric and neonatal immune responses | Pediatric Research (nature.com)
Biggio, J. et al. (2015) ‘9: Neonatal, not maternal, copy number variants are associated with spontaneous preterm birth’, American Journal of Obstetrics and Gynecology, 212(1), p. S8: 9: Neonatal, not maternal, copy number variants are associated with spontaneous preterm birth - American Journal of Obstetrics & Gynecology (ajog.org)
Bozack, A.K. et al. (2018) ‘DNA methylation in cord blood as mediator of the association between prenatal arsenic exposure and gestational age’, Epigenetics, 13(9), pp. 923–940. Available at: https://doi.org/10.1080/15592294.2018.1516453
Bozack, A.K. et al. (2020) ‘Cord blood DNA methylation of DNMT3A mediates the association between in utero arsenic exposure and birth outcomes: Results from a prospective birth cohort in Bangladesh’, Environmental Research, 183, p. 109134: https://doi.org/10.1016/j.envres.2020.109134
Bozack, A.K. et al. (2022) ‘The impact of prenatal and early-life arsenic exposure on epigenetic age acceleration among adults in Northern Chile’, Environmental Epigenetics, 8(1), p. dvac014: https://doi.org/10.1093/eep/dvac014
Cardenas, A. et al. (2015) ‘Arsenic Exposure and Prevalence of the Varicella Zoster Virus in the United States: NHANES (2003–2004 and 2009–2010)’, Environmental Health Perspectives, 123(6), pp. 590–596: https://doi.org/10.1289/ehp.1408731
Centre for Disease Control and Prevention (2022) What is Epigenetics?: What is Epigenetics? | CDC
Chakraborty, A. et al. (2022) ‘Epigenetic modifications from arsenic exposure: A comprehensive review’, Science of The Total Environment, 810, p. 151218: https://doi.org/10.1016/j.scitotenv.2021.151218
Cheikhi, A. et al. (2020) ‘Arsenic Stimulates Myoblast Mitochondrial Epidermal Growth Factor Receptor to Impair Myogenesis’, Toxicological Sciences, 176(1), pp. 162–174: Arsenic Stimulates Myoblast Mitochondrial Epidermal Growth Factor Receptor to Impair Myogenesis | Toxicological Sciences | Oxford Academic (oup.com)
Chen, C. et al. (2017) ‘MicroRNA-155 regulates arsenite-induced malignant transformation by targeting Nrf2-mediated oxidative damage in human bronchial epithelial cells’, Toxicology Letters, 278, pp. 38–47: https://doi.org/10.1016/j.toxlet.2017.07.215
Chen, Q.Y. et al. (2018) ‘Role of miR-31 and SATB2 in arsenic-induced malignant BEAS-2B cell transformation’, Molecular Carcinogenesis, 57(8), pp. 968–977: https://doi.org/10.1002/mc.22817
Cheng, H. et al. (2018) ‘Relative miRNA and mRNA expression involved in arsenic methylation’, PLOS ONE. Edited by B.-H. Jiang, 13(12), p. e0209014: https://doi.org/10.1371/journal.pone.0209014
Chicoine, É. et al. (2002) ‘Evidence for the role of promoter methylation in the regulation of MMP-9 gene expression’, Biochemical and Biophysical Research Communications, 297(4), pp. 765–772: https://doi.org/10.1016/S0006-291X(02)02283-0
Cobo, J.M., Valdez, J.G. and Gurley, L.R. (1995) ‘Inhibition of mitotic-specific histone phosphorylation by sodium arsenite’, Toxicology in Vitro, 9(4), pp. 459–465: https://doi.org/10.1016/0887-2333(95)00038-A
Cronican, A.A. et al. (2013) ‘Genome-Wide Alteration of Histone H3K9 Acetylation Pattern in Mouse Offspring Prenatally Exposed to Arsenic’, PLoS ONE. Edited by R. Johnson, 8(2), p. e53478: https://doi.org/10.1371/journal.pone.0053478
Dai, L. et al. (2020) ‘Elevated whole blood arsenic level is associated with type 2 diabetes in coal-burning areas in Guizhou’, Toxicology and Applied Pharmacology, 403, p. 115135: https://doi.org/10.1016/j.taap.2020.115135
Demanelis, K. et al. (2019) ‘Association of Arsenic Exposure with Whole Blood DNA Methylation: An Epigenome-Wide Study of Bangladeshi Adults’, Environmental Health Perspectives, 127(5), p. 057011: https://doi.org/10.1289/EHP3849
Deyssenroth, M.A. et al. (2022) ‘Placental Gene Transcript Proportions are Altered in the Presence of In Utero Arsenic and Cadmium Exposures, Genetic Variants, and Birth Weight Differences’, Frontiers in Genetics, 13, p. 865449: Frontiers | Placental Gene Transcript Proportions are Altered in the Presence of In Utero Arsenic and Cadmium Exposures, Genetic Variants, and Birth Weight Differences (frontiersin.org)
Domingo-Relloso, A. et al. (2022) ‘Arsenic Exposure, Blood DNA Methylation, and Cardiovascular Disease’, Circulation Research, 131(2): https://doi.org/10.1161/CIRCRESAHA.122.320991
Du, X. et al. (2018) ‘Cortex and hippocampus DNA epigenetic response to a long-term arsenic exposure via drinking water’, Environmental Pollution, 234, pp. 590–600: https://doi.org/10.1016/j.envpol.2017.11.083
EFSA CONTAM (2009) ‘Scientific Opinion on Arsenic in Food’, EFSA Journal, 7(10), p. 1351: https://doi.org/10.1016/j.envpol.2017.11.083
Eick, S.M. et al. (2019) ‘Socioeconomic status and the association between arsenic exposure and type 2 diabetes’, Environmental Research, 172, pp. 578–585: https://doi.org/10.1016/j.envres.2019.03.013
FERA (2015) ‘Total Diet Study of metals and other elements in food’, pp. 1–69.
Fry, R.C. et al. (2007) ‘Activation of inflammation/NF-kappaB signaling in infants born to arsenic-exposed mothers’, PLoS genetics, 3(11), p. e207: https://doi.org/10.1371/journal.pgen.0030207
Gangopadhyay, S. et al. (2019) ‘Potential facet for prenatal arsenic exposure paradigm: linking endocrine disruption and epigenetics’, The Nucleus, 62(2), pp. 127–142: Potential facet for prenatal arsenic exposure paradigm: linking endocrine disruption and epigenetics | SpringerLink
Genchi, G. et al. (2022) ‘Arsenic: A Review on a Great Health Issue Worldwide’, Applied Sciences, 12(12), p. 6184: https://doi.org/10.3390/app12126184
George, S. et al. (2023) ‘Epigenomic reprogramming in iAs-mediated carcinogenesis’, in Advances in Pharmacology. Elsevier, pp. 319–365: https://doi.org/10.1016/bs.apha.2022.08.004
Gonzalez, H. et al. (2015) ‘Arsenic-exposed Keratinocytes Exhibit Differential microRNAs Expression Profile; Potential Implication of miR-21, miR-200a and miR-141 in Melanoma Pathway’, Clinical Cancer Drugs, 2(2), pp. 138–147: Arsenic-exposed Keratinocytes Exhibit Differential microRNAs Expression Profile; Potential Implication of miR-21, miR-200a and miR-141 in Melanoma Pathway | Bentham Science (eurekaselect.com)
Gonzalez-Cortes, T. et al. (2017) ‘DNA methylation of extracellular matrix remodeling genes in children exposed to arsenic’, Toxicology and Applied Pharmacology, 329, pp. 140–147: https://doi.org/10.1016/j.taap.2017.06.001
Grau-Pérez, M. et al. (2017) ‘The Association of Arsenic Exposure and Metabolism With Type 1 and Type 2 Diabetes in Youth: The SEARCH Case-Control Study’, Diabetes Care, 40(1), pp. 46–53: https://doi.org/10.2337/dc16-0810
Guo, P. et al. (2020) ‘SFPQ is involved in regulating arsenic-induced oxidative stress by interacting with the miRNA-induced silencing complexes’, Environmental Pollution, 261, p. 114160: https://doi.org/10.1016/j.envpol.2020.114160
He, J. et al. (2014) ‘Chronic Arsenic Exposure and Angiogenesis in Human Bronchial Epithelial Cells via the ROS/miR-199a-5p/HIF-1 α /COX-2 Pathway’, Environmental Health Perspectives, 122(3), pp. 255–261: https://doi.org/10.1289/ehp.1307545
He, J. et al. (2019) ‘Arsenic-induced metabolic shift triggered by the loss of miR-199a-5p through Sp1-dependent DNA methylation’, Toxicology and Applied Pharmacology, 378, p. 114606: https://doi.org/10.1016/j.taap.2019.114606
Hossain, K. et al. (2017) ‘Chronic exposure to arsenic, LINE-1 hypomethylation, and blood pressure: a cross-sectional study in Bangladesh’, Environmental Health, 16(1), p. 20: https://doi.org/10.1186/s12940-017-0231-7
Hu, L. et al. (2017) ‘Arsenic-induced sumoylation of Mus81 is involved in regulating genomic stability’, Cell Cycle, 16(8), pp. 802–811: https://doi.org/10.1080/15384101.2017.1302628
IARC (2018) ‘Arsenic and Arsenic Compounds’, pp. 1–54.
Intarasunanont, P. et al. (2012) ‘Effects of arsenic exposure on DNA methylation in cord blood samples from newborn babies and in a human lymphoblast cell line’, Environmental Health, 11(1), p. 31: https://doi.org/10.1186/1476-069X-11-3
Islam, R. et al. (2022) ‘Epigenetic Dysregulations in Arsenic-Induced Carcinogenesis’, Cancers, 14(18), p. 4502: https://doi.org/10.3390/cancers14184502
Jo, W.J. et al. (2009) ‘Acetylated H4K16 by MYST1 protects UROtsa cells from arsenic toxicity and is decreased following chronic arsenic exposure’, Toxicology and Applied Pharmacology, 241(3), pp. 294–302: https://doi.org/10.1016/j.taap.2009.08.027
Kaushal, A. et al. (2017) ‘Genome-wide DNA methylation at birth in relation to in utero arsenic exposure and the associated health in later life’, Environmental Health, 16(1), p. 50: https://doi.org/10.1186/s12940-017-0262-0
Khan, F. et al. (2017) ‘Epigenetic mechanisms underlying the toxic effects associated with arsenic exposure and the development of diabetes’, Food and Chemical Toxicology, 107, pp. 406–417: https://doi.org/10.1016/j.fct.2017.07.021
Kile, M.L. et al. (2012) ‘Prenatal Arsenic Exposure and DNA Methylation in Maternal and Umbilical Cord Blood Leukocytes’, Environmental Health Perspectives, 120(7), pp. 1061–1066: https://doi.org/10.1289/ehp.1104173
Kitchin, K.T. and Conolly, R. (2010) ‘Arsenic-Induced Carcinogenesis—Oxidative Stress as a Possible Mode of Action and Future Research Needs for More Biologically Based Risk Assessment’, Chemical Research in Toxicology, 23(2), pp. 327–335: https://doi.org/10.1021/tx900343d
Koestler, D.C. et al. (2013) ‘Differential DNA Methylation in Umbilical Cord Blood of Infants Exposed to Low Levels of Arsenic in Utero’, Environmental Health Perspectives, 121(8), pp. 971–977: https://doi.org/10.1289/ehp.1205925
Laine, J.E. and Fry, R.C. (2016) ‘A Systems Toxicology-based Approach Reveals Biological Pathways Dysregulated by Prenatal Arsenic Exposure’, Annals of Global Health, 82(1), p. 189: A Systems Toxicology-based Approach Reveals Biological Pathways Dysregulated by Prenatal Arsenic Exposure - Annals of Global Health
Langfelder, P. and Horvath, S. (2007) ‘Eigengene networks for studying the relationships between co-expression modules.’, BMC Systems Biology, (1), p. 54: https://doi.org/10.1186/1752-0509-1-54
Levine, M.E. et al. (2018) ‘An epigenetic biomarker of aging for lifespan and healthspan’, Aging, 10(4), pp. 573–591: https://doi.org/10.18632/aging.101414
Li, J. et al. (2002) ‘Arsenic Trioxide Promotes Histone H3 Phosphoacetylation at the Chromatin of CASPASE-10 in Acute Promyelocytic Leukemia Cells’, Journal of Biological Chemistry, 277(51), pp. 49504–49510: https://doi.org/10.1074/jbc.M207836200
Ling, M. et al. (2012) ‘Regulation of miRNA-21 by reactive oxygen species-activated ERK/NF-κB in arsenite-induced cell transformation’, Free Radical Biology and Medicine, 52(9), pp. 1508–1518: https://doi.org/10.1016/j.freeradbiomed.2012.02.020
Liu, D. et al. (2015) ‘Arsenic Trioxide Reduces Global Histone H4 Acetylation at Lysine 16 through Direct Binding to Histone Acetyltransferase hMOF in Human Cells’, PLOS ONE. Edited by T. Thomas, 10(10), p. e0141014: https://doi.org/10.1371/journal.pone.0141014
Liu, J. et al. (2020) ‘The Mechanism of Trivalent Inorganic Arsenic on HIF-1α: a Systematic Review and Meta-analysis’, Biological Trace Element Research, 198(2), pp. 449–463: https://doi.org/10.1007/s12011-020-02087-x
Liu, J.-T. and Bain, L.J. (2018) ‘Arsenic Induces Members of the mmu-miR-466-669 Cluster Which Reduces NeuroD1 Expression’, Toxicological Sciences, 162(1), pp. 64–78: https://doi.org/10.1093/toxsci/kfx241
Liu, S. et al. (2015) ‘Arsenite Targets the Zinc Finger Domains of Tet Proteins and Inhibits Tet-Mediated Oxidation of 5-Methylcytosine’, Environmental Science & Technology, 49(19), pp. 11923–11931: https://doi.org/10.1021/acs.est.5b03386
Liu, X. et al. (2016) ‘MicroRNA-21 activation of ERK signaling via PTEN is involved in arsenite-induced autophagy in human hepatic L-02 cells’, Toxicology Letters, 252, pp. 1–10: https://doi.org/10.1016/j.toxlet.2016.04.015
Lo, W.-S. et al. (2000) ‘Phosphorylation of Serine 10 in Histone H3 Is Functionally Linked In Vitro and In Vivo to Gcn5-Mediated Acetylation at Lysine 14’, Molecular Cell, 5(6), pp. 917–926: https://doi.org/10.1016/S1097-2765(00)80257-9
Luo, F. et al. (2013) ‘Arsenite evokes IL-6 secretion, autocrine regulation of STAT3 signaling, and miR-21 expression, processes involved in the EMT and malignant transformation of human bronchial epithelial cells’, Toxicology and Applied Pharmacology, 273(1), pp. 27–34: https://doi.org/10.1016/j.taap.2013.08.025
Luo, F. et al. (2015) ‘MicroRNA-21, up-regulated by arsenite, directs the epithelial–mesenchymal transition and enhances the invasive potential of transformed human bronchial epithelial cells by targeting PDCD4’, Toxicology Letters, 232(1), pp. 301–309: https://doi.org/10.1016/j.toxlet.2014.11.001
Luvonga, C. et al. (2020) ‘Organoarsenicals in Seafood: Occurrence, Dietary Exposure, Toxicity, and Risk Assessment Considerations – A Review’, Journal of Agricultural and Food Chemistry, 68(4), pp. 943–960: https://doi.org/10.1021/acs.jafc.9b07532
Ma, L. et al. (2016) ‘Specific histone modification responds to arsenic-induced oxidative stress’, Toxicology and Applied Pharmacology, 302, pp. 52–61: https://doi.org/10.1016/j.taap.2016.03.015
Martinez, V.D. and Lam, W.L. (2021) ‘Health Effects Associated With Pre- and Perinatal Exposure to Arsenic’, Frontiers in Genetics, 12, p. 664717: https://doi.org/10.3389/fgene.2021.664717
Martinez-Zamudio, R. and Ha, H.C. (2011) ‘Environmental epigenetics in metal exposure’, Epigenetics, 6(7), pp. 820–827: https://doi.org/10.4161/epi.6.7.16250
Maull, E.A. et al. (2012) ‘Evaluation of the Association between Arsenic and Diabetes: A National Toxicology Program Workshop Review’, Environmental Health Perspectives, 120(12), pp. 1658–1670: https://doi.org/10.1289/ehp.1104579
Meng, X.-Z. et al. (2011) ‘microRNA expression alteration after arsenic trioxide treatment in HepG-2 cells: Role of microRNA in arsenic trioxide’, Journal of Gastroenterology and Hepatology, 26(1), pp. 186–193: https://doi.org/10.1111/j.1440-1746.2010.06317.x
Michailidi, C. et al. (2015) ‘Involvement of Epigenetics and EMT-Related miRNA in Arsenic-Induced Neoplastic Transformation and Their Potential Clinical Use’, Cancer Prevention Research, 8(3), pp. 208–221: https://doi.org/10.1158/1940-6207.CAPR-14-0251
Minatel, B.C. et al. (2018) ‘Environmental arsenic exposure: From genetic susceptibility to pathogenesis’, Environment International, 112, pp. 183–197: https://doi.org/10.1016/j.envint.2017.12.017
Muka, T. et al. (2016) ‘The role of epigenetic modifications in cardiovascular disease: A systematic review’, International Journal of Cardiology, 212, pp. 174–183: https://doi.org/10.1016/j.ijcard.2016.03.062
Ngalame, N.N.O. et al. (2016) ‘Mitigation of arsenic-induced acquired cancer phenotype in prostate cancer stem cells by miR-143 restoration’, Toxicology and Applied Pharmacology, 312, pp. 11–18: https://doi.org/10.1016/j.taap.2015.12.013
Nohara, K. et al. (2012) ‘Late-onset Increases in Oxidative Stress and Other Tumorigenic Activities and Tumors With a Ha-ras Mutation in the Liver of Adult Male C3H Mice Gestationally Exposed to Arsenic’, Toxicological Sciences, 129(2), pp. 293–304: https://doi.org/10.1093/toxsci/kfs203
Nohara, K. et al. (2020) ‘Gestational arsenic exposure induces site-specific DNA hypomethylation in active retrotransposon subfamilies in offspring sperm in mice’, Epigenetics & Chromatin, 13(1), p. 53: https://doi.org/10.1186/s13072-020-00375-3
Olmedo-Suárez, M.Á. et al. (2022) ‘Epigenetic Regulation in Exposome-Induced Tumorigenesis: Emerging Roles of ncRNAs’, Biomolecules, 12(4), p. 513: https://doi.org/10.3390/biom12040513
Ouyang, Y. et al. (2020) ‘S‐adenosylmethionine: A metabolite critical to the regulation of autophagy’, Cell Proliferation, 53(11), p. e12891: https://doi.org/10.1111/cpr.12891
Paul, S. et al. (2014) ‘Arsenic-induced promoter hypomethylation and over-expression of ERCC2 reduces DNA repair capacity in humans by non-disjunction of the ERCC2–Cdk7 complex’, Metallomics, 6(4), p. 864: https://doi.org/10.1039/c3mt00328k
Pilsner, J.R. et al. (2012) ‘Influence of Prenatal Arsenic Exposure and Newborn Sex on Global Methylation of Cord Blood DNA’, PLoS ONE. Edited by C. Oudejans, 7(5), p. e37147: https://doi.org/10.1371/journal.pone.0037147
Pournara, A. et al. (2016) ‘Arsenic alters global histone modifications in lymphocytes in vitro and in vivo’, Cell Biology and Toxicology, 32(4), pp. 275–284: https://doi.org/10.1007/s10565-016-9334-0
Prigent, C. and Dimitrov, S. (2003) ‘Phosphorylation of serine 10 in histone H3, what for?’, Journal of Cell Science, 116(18), pp. 3677–3685: https://doi.org/10.1242/jcs.00735
Rafiei, G. et al. (2019) ‘The Impact of Long-term Exposure to Low Levels of Inorganic Arsenic on the Hypomethylation of SEPT9 Promoter in Epithelial-Mesenchymal Transformed Colorectal Cancer Cell Lines’, International Journal of Molecular and Cellular Medicine, 8(2): https://doi.org/10.22088/IJMCM.BUMS.8.2.130
Rager, J.E. et al. (2014) ‘Prenatal arsenic exposure and the epigenome: Altered microRNAs associated with innate and adaptive immune signaling in newborn cord blood’, Environmental and Molecular Mutagenesis, 55(3), pp. 196–208: https://doi.org/10.1002/em.21842
Rager, J.E. et al. (2017) ‘Benchmark Dose Modeling Estimates of the Concentrations of Inorganic Arsenic That Induce Changes to the Neonatal Transcriptome, Proteome, and Epigenome in a Pregnancy Cohort’, Chemical Research in Toxicology, 30(10), pp. 1911–1920: https://doi.org/10.1021/acs.chemrestox.7b00221
Ratnaike, R.N. (2003) ‘Acute and chronic arsenic toxicity’, Postgraduate Medical Journal, 79(933), pp. 391–396: https://doi.org/10.1136/pmj.79.933.391
Ray, P.D., Huang, B.-W. and Tsuji, Y. (2015) ‘Coordinated regulation of Nrf2 and histone H3 serine 10 phosphorylation in arsenite-activated transcription of the human heme oxygenase-1 gene’, Biochimica et Biophysica Acta (BBA) - Gene Regulatory Mechanisms, 1849(10), pp. 1277–1288: https://doi.org/10.1016/j.bbagrm.2015.08.004
Rea, M. et al. (2017) ‘Genome-wide DNA methylation reprogramming in response to inorganic arsenic links inhibition of CTCF binding, DNMT expression and cellular transformation’, Scientific Reports, 7(1), p. 41474: https://doi.org/10.1038/srep41474
Reichard, J.F. and Puga, A. (2010) ‘Effects of arsenic exposure on DNA methylation and epigenetic gene regulation’, Epigenomics, 2(1), pp. 87–104: https://doi.org/10.2217/epi.09.45
Rojas, D. et al. (2015) ‘Prenatal Arsenic Exposure and the Epigenome: Identifying Sites of 5-methylcytosine Alterations that Predict Functional Changes in Gene Expression in Newborn Cord Blood and Subsequent Birth Outcomes’, Toxicological Sciences, 143(1), pp. 97–106: https://doi.org/10.1093/toxsci/kfu210
Rossetto, D., Avvakumov, N. and Côté, J. (2012) ‘Histone phosphorylation: A chromatin modification involved in diverse nuclear events’, Epigenetics, 7(10), pp. 1098–1108: https://doi.org/10.4161/epi.21975
SACN (2011) ‘The influence of maternal, fetal and child nutrition on the development of chronic disease in later life’, pp. 1–192.
SACN (2018) ‘Feeding in the First Year of Life’, pp. 1–271.
Sanyal, T. et al. (2018) ‘Hypomethylation of mitochondrial D-loop and ND6 with increased mitochondrial DNA copy number in the arsenic-exposed population’, Toxicology, 408, pp. 54–61: https://doi.org/10.1016/j.tox.2018.06.012
Simeonova, P.P. and Luster, M.I. (2000) ‘Mechanisms of arsenic carcinogenicity: genetic or epigenetic mechanisms?’, Journal of Environmental Pathology, Toxicology and Oncology: Official Organ of the International Society for Environmental Toxicology and Cancer, 19(3), pp. 281–286.
Sitras, V. et al. (2009) ‘Placental Gene Expression Profile in Intrauterine Growth Restriction Due to Placental Insufficiency’, Reproductive Sciences, 16(7), pp. 701–711: https://doi.org/10.1177/1933719109334256
Smeester, L. et al. (2011) ‘Epigenetic Changes in Individuals with Arsenicosis’, Chemical Research in Toxicology, 24(2), pp. 165–167: https://doi.org/10.1021/tx1004419
Smeester, L. et al. (2017) ‘Toxic metals in amniotic fluid and altered gene expression in cell-free fetal RNA’, Prenatal Diagnosis, 37(13), pp. 1364–1366: https://doi.org/10.1002/pd.5183
Smeester, L. and Fry, R.C. (2018) ‘Long-Term Health Effects and Underlying Biological Mechanisms of Developmental Exposure to Arsenic’, Current Environmental Health Reports, 5(1), pp. 134–144: https://doi.org/10.1007/s40572-018-0184-1
Suzuki, T. et al. (2009) ‘Trivalent dimethylarsenic compound induces histone H3 phosphorylation and abnormal localization of Aurora B kinase in HepG2 cells’, Toxicology and Applied Pharmacology, 241(3), pp. 275–282: https://doi.org/10.1016/j.taap.2009.08.017
Suzuki, T., Kita, K. and Ochi, T. (2013) ‘Phosphorylation of histone H3 at serine 10 has an essential role in arsenite-induced expression of FOS , EGR1 and IL8 mRNA in cultured human cell lines: Histone H3 phosphorylation and gene regulation by iAs(III)’, Journal of Applied Toxicology, 33(8), pp. 746–755 https://doi.org/10.1002/jat.2724
The Royal Society of Chemistry (2023) Arsenic, Arsenic: Arsenic - Element information, properties and uses | Periodic Table (rsc.org) (Accessed: 10 January 2023).
Thomas, D.J. (2021) ‘Arsenic methylation – Lessons from three decades of research’, Toxicology, 457, p. 152800: https://doi.org/10.1016/j.tox.2021.152800
Vaiserman, A. and Lushchak, O. (2021) ‘DNA methylation changes induced by prenatal toxic metal exposure: An overview of epidemiological evidence’, Environmental Epigenetics, 7(1), p. dvab007: https://doi.org/10.1093/eep/dvab007
Waalkes, M.P. et al. (2004) ‘Estrogen Signaling in Livers of Male Mice With Hepatocellular Carcinoma Induced by Exposure to Arsenic In Utero’, JNCI Journal of the National Cancer Institute, 96(6), pp. 466–474: https://doi.org/10.1093/jnci/djh070
Wang, M. et al. (2016) ‘Role and mechanism of miR-222 in arsenic-transformed cells for inducing tumor growth’, Oncotarget, 7(14), pp. 17805–17814: https://doi.org/10.18632/oncotarget.7525
Wang, Z. et al. (2011) ‘Reversal and Prevention of Arsenic-Induced Human Bronchial Epithelial Cell Malignant Transformation by microRNA-200b’, Toxicological Sciences, 121(1), pp. 110–122: https://doi.org/10.1093/toxsci/kfr029
Wang, Z. et al. (2014) ‘MicroRNA-200b Suppresses Arsenic-transformed Cell Migration by Targeting Protein Kinase Cα and Wnt5b-Protein Kinase Cα Positive Feedback Loop and Inhibiting Rac1 Activation’, Journal of Biological Chemistry, 289(26), pp. 18373–18386: https://doi.org/10.1074/jbc.M114.554246
Winterbottom, E.F., Moroishi, Y., et al. (2019) ‘Prenatal arsenic exposure alters the placental expression of multiple epigenetic regulators in a sex-dependent manner’, Environmental Health, 18(1), p. 18: Prenatal arsenic exposure alters the placental expression of multiple epigenetic regulators in a sex-dependent manner | Environmental Health | Full Text (biomedcentral.com)
Winterbottom, E.F., Ban, Y., et al. (2019) ‘Transcriptome-wide analysis of changes in the fetal placenta associated with prenatal arsenic exposure in the New Hampshire Birth Cohort Study’, Environmental Health, 18(1), p. 100: Transcriptome-wide analysis of changes in the fetal placenta associated with prenatal arsenic exposure in the New Hampshire Birth Cohort Study | Environmental Health | Full Text (biomedcentral.com)
Yang, F. and Zhang, A. (2022) ‘Role of N6 ‐methyladenosine RNA modification in the imbalanced inflammatory homeostasis of arsenic‐induced skin lesions’, Environmental Toxicology, 37(8), pp. 1831–1839: https://doi.org/10.1002/tox.23530
Zeng, Q. et al. (2019) ‘Association and risk of five miRNAs with arsenic-induced multiorgan damage’, Science of The Total Environment, 680, pp. 1–9: https://doi.org/10.1016/j.scitotenv.2019.05.042
Zhang, S. et al. (2016) ‘Arsenic trioxide suppresses cell growth and migration via inhibition of miR-27a in breast cancer cells’, Biochemical and Biophysical Research Communications, 469(1), pp. 55–61: https://doi.org/10.1016/j.bbrc.2015.11.071
Zhang, Y. (2003) ‘Transcriptional regulation by histone ubiquitination and deubiquitination’, Genes & Development, 17(22), pp. 2733–2740: Transcriptional regulation by histone ubiquitination and deubiquitination (cshlp.org)
Zhao, T. et al. (2023) ‘N6-methyladenosine upregulates ribosome biogenesis in environmental carcinogenesis’, Science of The Total Environment, 881, p. 163428: https://doi.org/10.1016/j.scitotenv.2023.163428
Zhong, M. et al. (2018) ‘Malignant Transformation of Human Bronchial Epithelial Cells Induced by Arsenic through STAT3/miR-301a/SMAD4 Loop’, Scientific Reports, 8(1), p. 13291: Malignant Transformation of Human Bronchial Epithelial Cells Induced by Arsenic through STAT3/miR-301a/SMAD4 Loop | Scientific Reports (nature.com)
Zhou, X. et al. (2008) ‘Arsenite alters global histone H3 methylation’, Carcinogenesis, 29(9), pp. 1831–1836: https://doi.org/10.1093/carcin/bgn063
Zhou, X. et al. (2009) ‘Effects of nickel, chromate, and arsenite on histone 3 lysine methylation’, Toxicology and Applied Pharmacology, 236(1), pp. 78–84. https://doi.org/10.1016/j.taap.2009.01.009
Appendices
Appendix 1: Names and Abbreviations for Arsenic Species (EFSA CONTAM, 2009)
Table 11: List of names, abbreviations, and comments for different As species.
|
Name |
Abbreviation |
Comment |
|
Inorganic arsenic |
iAs |
The total sum of As(III) and As(V). |
|
Arsenite |
As(III) |
Highly toxic compound found at low levels in most foods. |
|
Arsenate |
As(V) |
Highly toxic compound that is found at trace to low levels in foods. |
|
Arsenobetaine |
AB |
Non-toxic arsenic species abundant in most seafoods. |
|
Arsenocholine |
AC |
Found in seafood at trace levels. This species of As is readily oxidised to AB in biological systems. |
|
Arsenosugars |
N/A |
Abundant arsenic species found in seafoods. |
|
Arsenolipids |
N/A |
Arsenic species found in fatty fish and fish oils. |
|
Arsenic containing fatty acids |
AsFA |
Group of fat soluble arsenic species present in fish and seafood. |
|
Arsenic containing hydrocarbons |
AsHC |
One of the groups of arsenolipids. |
|
Methylarsonate |
MA(V) |
A metabolite of As found in human urine. Found in trace levels in seafood and terrestrial foods. |
|
Methylarsonite |
MA(III) |
A toxic metabolite of iAs found in human urine. Species not normally detected in foods. |
|
Methylarsenate |
MA |
N/A |
|
Dimethylarsinate |
DMA(V) |
Minor arsenic species in seafoods and some terrestrial foods; the major human urine metabolite of iAs, arsenosugars and arsenolipids. |
|
Dimethylarsinite |
DMA(III) |
An unstable, reactive metabolite of iAs found in human urine. Species not normally detected in foods as difficult to measure due to its instability. Species is highly toxic. |
|
Dimethylmonoarsenate |
DMA |
N/A |
|
Methylarsonous acid |
MMA(III) |
N/A |
|
Methylarsonic acid |
MAA(V) |
N/A |
|
Dimethylarsinous acid |
DMAA(III) |
N/A |
|
Dimethylarsinic acid |
DMAA(V) |
N/A |
|
Dimethylarsonic acid |
DMMAA(III) |
N/A |
|
Trimethylarsine oxide |
TMAO |
Arsenic species found in seafood. |
|
Tetramethylarsonium ion |
TETRA |
Arsenic species found in seafood. |
|
Trimethylarsonio propionate |
TMAP |
Arsenic species present in seafoods. |
|
Thio-dimethylarsinate |
Thio-DMA |
A metabolite of iAs and arsenosugars found in human urine. |
Appendix 2: Pathways of Arsenic Metabolism* (Thomas, 2021)
*Upper – conversion via challenger pathway. Lower – conversion via alternative pathway.
Appendix 3: Dietary Exposure from iAs and tAs using the TDS
The UK TDS is performed routinely to calculate trends in exposure and calculate background exposure of varying commodities in the diet. ‘The key principle of a TDS is that it is representative of the whole diet. It is different from many surveys in that foods are prepared as if for consumption (rather than being analysed as sold), before being pooled into groups prior to analysis. This TDS involved the purchase of 24 retail samples (one from each of the identified local authorities) for each of the 138 categories of foods established by the FSA (3312 individual samples in total)’ (FERA, 2015).
Table 12: Estimated iAs population-based exposure from food consumed by women of childbearing age using data obtained from the TDS.
|
Food Groups |
Mean iAs Exposure – LB to UB (µg/kg/day)* for Females 16-49 years |
P97.5 iAs Exposure – LB to UB (µg/kg/day)* for Females 16-49 years |
|
Bread |
0-0.012 |
0-0.031 |
|
Misc. Cereals |
0.027 |
0.076 |
|
Carcass meat |
0-0.0041 |
0-0.019 |
|
Offal |
0-0.00015 |
0-0.0026 |
|
Meat products |
0-0.0064 |
0-0.027 |
|
Poultry |
0-0.0093 |
0-0.033 |
|
Fish and seafood |
0-0.0044 |
0-0.021 |
|
Fats and oils |
0-0.0021 |
0-0.0064 |
|
Eggs |
0-0.0034 |
0-0.016 |
|
Sugars and confectionary |
0-0.0040 |
0-0.016 |
|
Green vegetables |
0-0.0067 |
0-0.028 |
|
Potatoes |
0.016 |
0.048 |
|
Other vegetables |
0-0.016 |
0-0.052 |
|
Canned vegetables |
0-0.0063 |
0-0.029 |
|
Fresh fruit |
0-0.014 |
0-0.054 |
|
Fruit products |
0-0.0092 |
0-0.051 |
|
Non-alcoholic beverages |
0-0.062 |
0-0.15 |
|
Milk |
0-0.0054 |
0-0.020 |
|
Dairy products |
0-0.0096 |
0-0.036 |
|
Nuts and seeds |
0-0.0010 |
0-0.0088 |
|
Alcoholic beverages |
0-0.005 |
0-0.033 |
|
Meat alternatives |
0-0.00057 |
0-0.0071 |
|
Snacks |
0-0.0013 |
0-0.006 |
|
Desserts |
0-0.0024 |
0-0.015 |
|
Condiments |
0-0.0060 |
0-0.023 |
|
Tap water only |
0-0.021 |
0-0.092 |
|
Bottled water still or carbonated |
0-0.0051 |
0-0.041 |
|
Total^ |
0.043-0.26 |
0.098-0.51 |
*Values have been rounded to two significant figures.
LB - Lower bound; UB - Upper bound.
^P97.5th total values were determined from a distribution of consumption of any combination of food / drink categories rather than by summation of the individual 97.5th percentiles values for each category.
Table 13: Estimated population based tAs exposure from food consumed by women of childbearing age using data obtained from the TDS (FERA, 2015).
|
Food Groups |
Mean tAs Exposure – LB to UB (µg/kg bw/day)* for Females 16-49 years |
P97.5 tAs Exposure – LB to UB (µg/kg bw/day)* for Females 16-49 years |
|
Bread |
0-0.006 |
0-0.015 |
|
Misc. Cereals |
0.018 |
0.053 |
|
Carcass meat |
0-0.0021 |
0-0.0094 |
|
Offal |
0-0.000077 |
0-0.0013 |
|
Meat products |
0-0.0016 |
0-0.0069 |
|
Poultry |
0.0062 |
0.022 |
|
Fish and seafood |
0.74 |
3.6 |
|
Fats and oils |
0-0.00052 |
0-0.0016 |
|
Eggs |
0-0.00085 |
0-0.0040 |
|
Sugars and confectionary |
0-0.001 |
0-0.004 |
|
Green vegetables |
0-0.0017 |
0-0.0069 |
|
Potatoes |
0-0.0066 |
0-0.019 |
|
Other vegetables |
0-0.0081 |
0-0.026 |
|
Canned vegetables |
0-0.0016 |
0-0.0073 |
|
Fresh fruit |
0-0.0070 |
0-0.027 |
|
Fruit products |
0-0.0023 |
0-0.013 |
|
Non-alcoholic beverages |
0-0.062 |
0-0.15 |
|
Milk |
0-0.0054 |
0-0.02 |
|
Dairy products |
0-0.0024 |
0-0.0090 |
|
Nuts and seeds |
0.00043 |
0.0037 |
|
Alcoholic beverages |
0-0.005 |
0-0.033 |
|
Meat alternatives |
0.00019 |
0.0024 |
|
Snacks |
0.0012 |
0.0055 |
|
Desserts |
0.00059 |
0.0038 |
|
Condiments |
0.0055 |
0.021 |
|
Tap water only |
0-0.0084 |
0-0.037 |
|
Bottled water still or carbonated |
0-0.0020 |
0-0.017 |
|
Total^ |
0.77-0.89 |
3.6-3.8 |
*Values have been rounded to two significant figures.
LB - Lower bound; UB - Upper bound.
^P97.5th total values were determined from a distribution of consumption of any combination of food / drink categories rather than by summation of the individual 97.5th percentiles values for each category.